Ambulances wait up to 8 hours to offload patients as ERs fill up
Paramedics are waiting with patients in their ambulances or in ER hallways for hours before they’re admitted. Meanwhile, they can’t go to the next 911 call.
This story is the latest installment in our YouTube series, "What's Brewing,” investigative reporter Jenna Bourne's series of homemade deep dives into important issues during the coronavirus pandemic. Click here to check out the series and subscribe to our YouTube channel: The Deeper Dive.
Bypass 'We're busy'
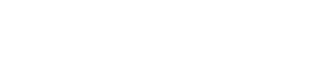
Tampa Bay area emergency rooms are so overwhelmed they’re telling ambulances to take their patients somewhere else.
Bay area paramedics are waiting with patients in their ambulances or in hallways for hours just to get them admitted to the ER.
“I am halfway through my shift, and this is probably, I don’t know, my 12th COVID patient so far today,” said Plant City ER nurse Candice Hughley, behind her mask and face shield.
She said it’s been like this every day while the delta variant surges in Florida.
“It’s been like we’re in a mass casualty disaster every single shift,” said Hughley. “We are out of beds, we are out of resources…I have ambulances sometimes that they’re just waiting in the hallway because I literally don’t have a stretcher to put a patient on. And that’s happening at every emergency room in the country.”


As ERs fill up, they go on “bypass.”
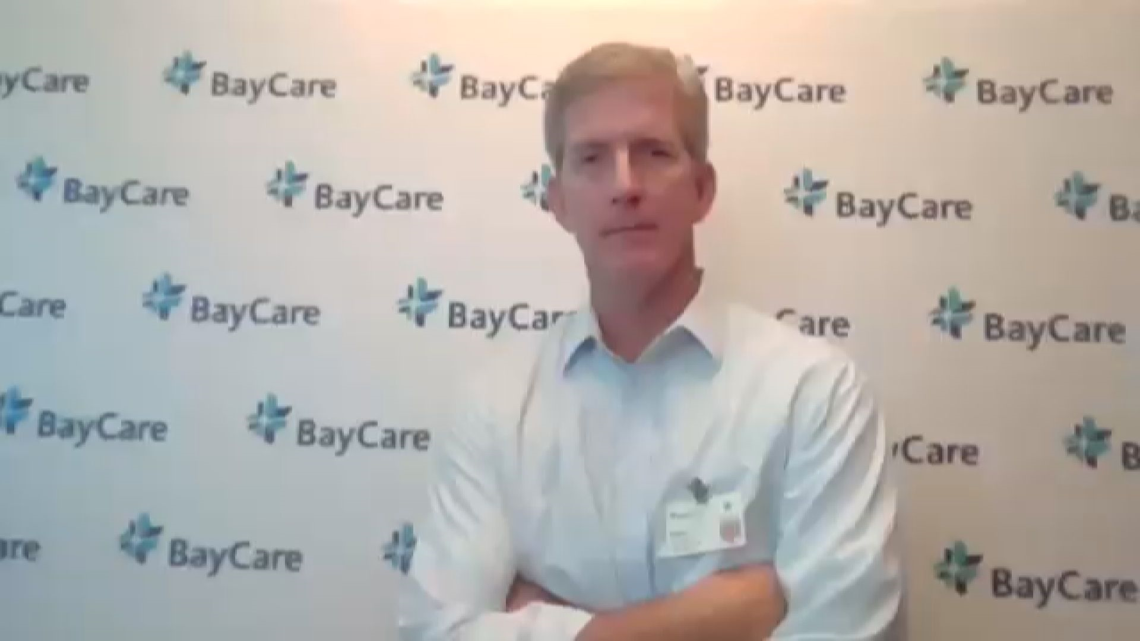
“Bypass or divert means we’re busy and we can’t see patients as soon as we would otherwise. So, that’s telling an ambulance take the patient to another hospital that’s not as busy,” said BayCare Chief Operating Officer and Executive Vice President Glenn Waters.
Florida Hospital Association President and CEO Mary Mayhew told 10 Investigates she’s never seen so many hospitals in the state on bypass before.
“No, this is incredibly unusual – to have this level of volume in our hospitals, in terms of maxed surge capacity,” said Mayhew.
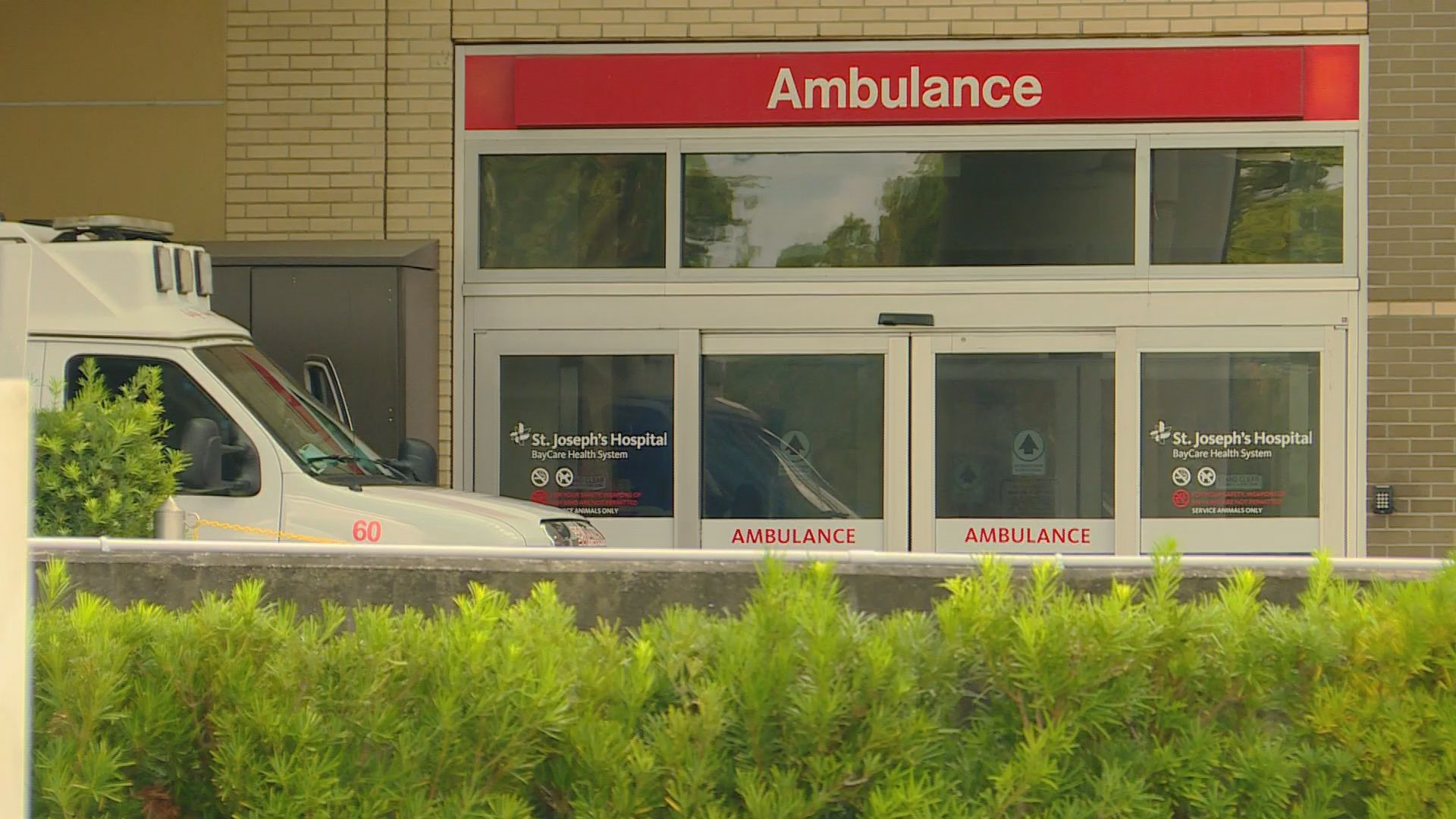
In Hillsborough County, bypass has become so common they launched an online bypass dashboard last month to help paramedics out in the field stay on top of where they can take their patients.
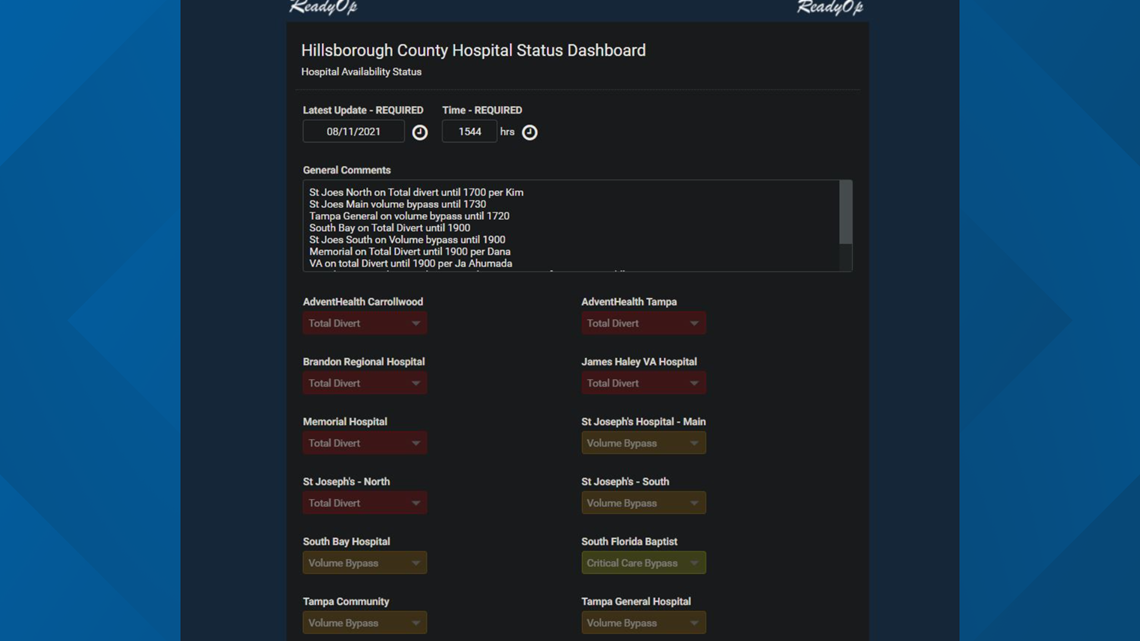
Before the online dashboard came out, Hillsborough County Fire Rescue Quality Management Chief Jeremy Fischler said hospitals and EMS communicated bypass status by phone.
“It relied heavily on landlines – phone calls being made between facilities, between EMS agencies,” said Fischler, who’s also the chair of the Hillsborough County Emergency Medical Planning Council’s Bypass Committee.
During the late afternoon on Aug. 11, Hillsborough County’s Hospital Status Dashboard showed a dire situation: All 12 hospital ERs in the county were on some form of bypass. Six were on “total divert,” meaning they were not accepting any new patients from ambulances.

“So, those ‘total divert’ facilities, because they provided us that status, they really are no longer an option because they’ve told us they are incapable. So, at that point, we just have to provide the highest level of care we can for a patient and get them to a facility that typically has the capabilities of taking care of that patient. When we get to those facilities, even though there may be a delay in them receiving definitive care from the ER staff, we still stand by the patient the entire time. We’re still monitoring that patient,” said Fischler.
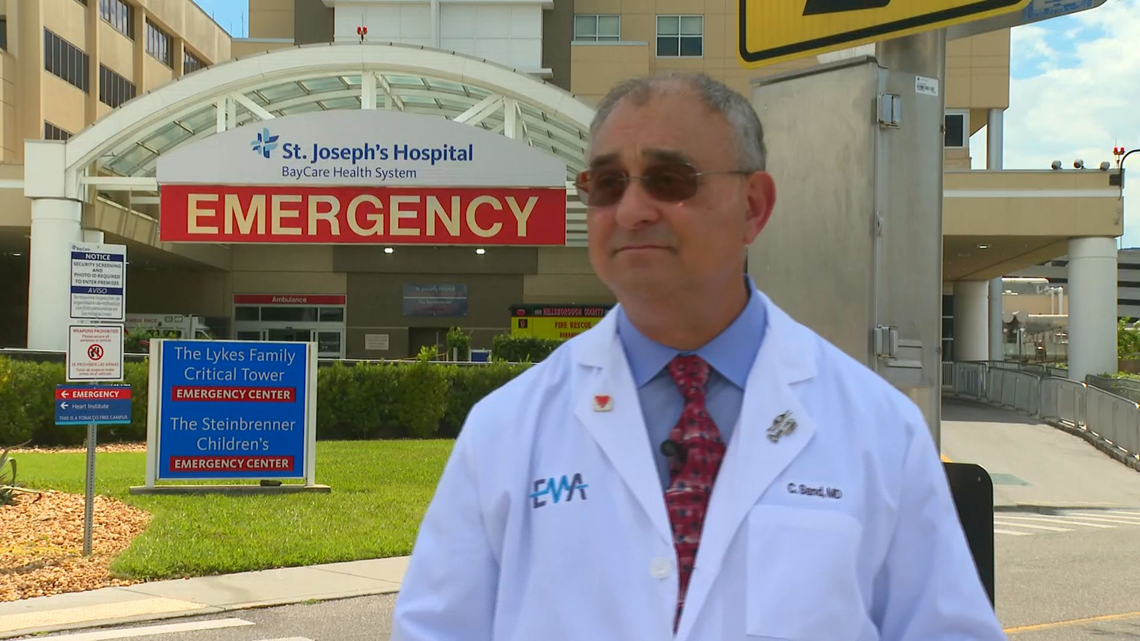
Dr. Charlie Sand, chair of Hillsborough’s Emergency Medical Planning Council, said this is happening all over.
“Our EMS system is absolutely overwhelmed. They’re waiting on the ramp, they’re waiting in the hallways to get beds. Sometimes, it’s several hours,” said Dr. Sand.
Fischler said Hillsborough County Fire Rescue’s data from the past month shows 301 patients waited more than 90 minutes from when their ambulance arrived at the ER to when they were admitted.
That was nearly 4 percent of patients transported in HCFR ambulances during that time.
Fischler said the longest wait was eight hours and four minutes.
Those ambulances, tied up for hours parked outside ERs while waiting to transfer patients, can’t go to the next 911 call.
“As you would expect, that does have an impact on response times and available resources. And it’s a negative impact,” said Fischler.

Dr. Sand said people should be concerned about what that means the next time they call 911.
“EMS might not be able to get to them on time,” said Dr. Sand.
Why now? Delta variant, staffing trouble, population boom
So, why is this happening? Experts boil it down to three main reasons.
Number one: The delta variant is more infectious, and it’s affecting younger patients.
“We’re seeing tons of people, unvaccinated, coming in sick and it’s just overwhelming our system right now,” said Dr. Sand.

Reason number two: Healthcare staffing shortages.
Mayhew said not only are hospital workers getting burnt out, many are taking travel nurse jobs – jobs with better pay that take them outside Florida.
“There has been a healthcare workforce shortage. That existed prior to the pandemic. Now, you add 17 months of the worst pandemic, where our nurses and respiratory therapists and ER staff have been on the frontlines confronting this incredible crisis – and the strain, the stress, the toll that that has taken on our healthcare staff,” said Mayhew.
Reason number three: More people are moving here.
“Our population has been exploding over the last several years and we just can’t keep up with the number of facilities to keep up with the increasing population,” said Fischler.
Our community’s emergency medical system is taking action to try to keep up.
Earlier this month, Hillsborough County Fire Rescue put four extra rescues in service.


Hospitals all over the Tampa Bay area tell us they’re converting spaces to make room for more COVID patients and postponing non-emergency elective surgeries, like hip replacements and hernia operations.
And Waters said going on divert and bypass is a strategy to make sure the sickest patients get the care they need.
“That is why we go on divert, to make sure we can take care of the people that really, really – the life and death situations where people really have an emergent condition. If we’re making people wait, it’s the ones that we’ve deemed aren’t as sick. And I hate to say it, but they can wait. Their condition is such that they can wait,” said Waters. “I heard the other day at one of the [BayCare] hospitals that we had patients waiting seven hours to be seen.”

You can help Consider alternatives to the ER
You can help lower the strain on our local ERs right now – and that’s aside from the obvious: Getting a vaccine, wearing a mask, social distancing.
If you need medical attention, but it’s not really an emergency, don’t go to the ER.
If you’re having a heart attack or a stroke, then yeah, go to the ER.
But if you have a rash, don’t go to the ER.
If you need to get tested for COVID, don’t go to the ER. Go to a pharmacy, urgent care, or a free county testing site.
“We need people to help take care of themselves and help us help them,” said Hughley.
Watch more from 'What's Brewing?' below:
REACH OUT: Got an episode idea? Email Jenna at jbourne@10tampabay.com. You can also like Jenna’s Facebook page and follow her on Twitter and Instagram.